
Your Cancer Screening Checklist
(It's More Than Mammograms)
October has us all thinking pink.
That’s important. Mammograms save lives. We want every woman to get screened.
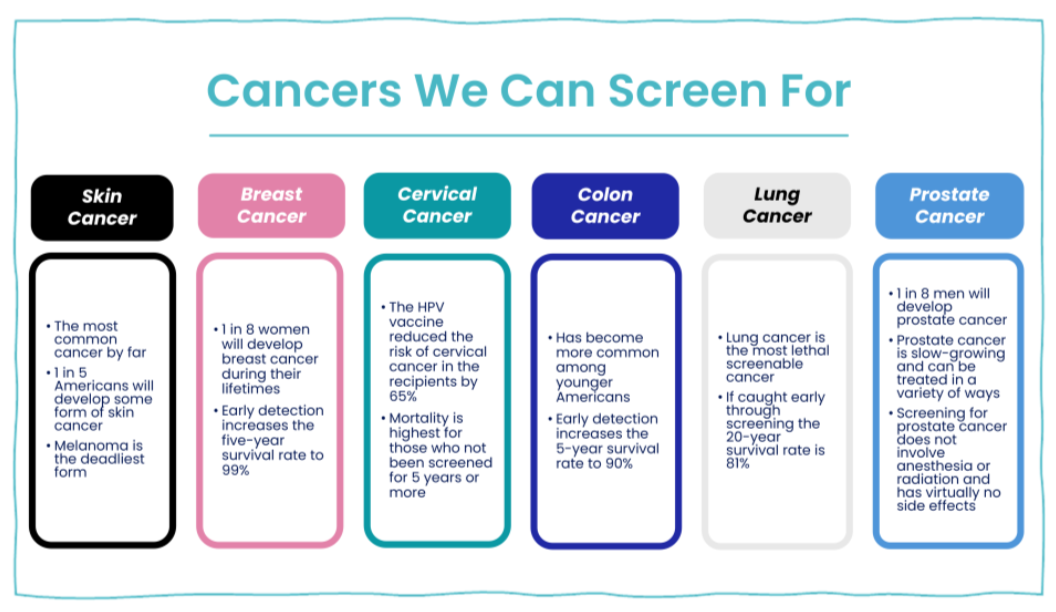
But we’ve been thinking, if October already has you thinking about cancer screenings, why stop at mammograms? There are six cancers we can find early through preventive screenings. That’s six chances to catch something when it’s most treatable.
Between 1991 and 2019, cancer deaths in the United States fell by 32%. That’s roughly 3.5 million lives saved. Three and a half million people, still here with their families, pursuing their dreams, and living their lives. That’s the power of catching cancer early.
The tricky part?
Guidelines keep changing. What age to start, how often, what’s covered by insurance; it can all be confusing.
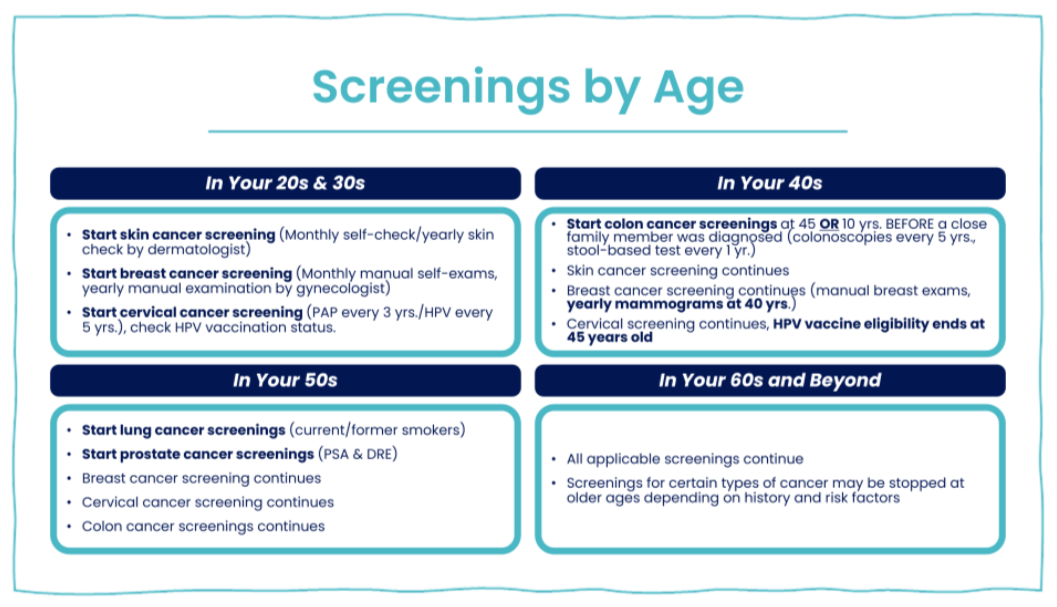
So, we did the homework for you. We looked at the latest recommendations from the American Cancer Society and the National Institutes of Health (NIH) to create a simple guide that shows which screenings you need and when.
But first, let’s talk about risk.
Understanding Your Risk
Not everyone’s risk looks the same. Some factors, like family history, genetics, or ethnicity, you can’t change. Others, like smoking, diet, and sun exposure, you can.
If you already know cancer runs in your family, don’t wait for your provider to bring it up. Tell them. Ask about starting preventive screening earlier.
A mother or sister with breast cancer? Don’t wait until 40 for your first mammogram.
A dad diagnosed with prostate cancer at 55? You might start at 45.
Ever smoked? Even years ago, ask about lung screening.
The timelines below are meant for people at average risk. If you think you’re at risk, that’s an important conversation to have with your provider so they can tailor a plan that fits you.
Your Cancer Screening Checklist
Skin Cancer
Skin cancer is the most common cancer in America; one in five of us will develop it. Melanoma is the deadliest type, but when found early, it’s one of the easiest cancers to treat.
Who’s at higher risk?
If you have fair skin that burns easily, light eyes or hair, a history of sunburns or tanning beds, or more than 50 freckles and moles, you’re more likely to develop it. Outdoor workers and anyone who’s had skin cancer before should be especially vigilant.
When to start screening:
Ask your provider for a yearly skin exam starting in your 20s or 30s and mention any new or changing moles right away. Between visits, do quick self-checks to look for new moles or ones with uneven edges or multiple colors. A few minutes in front of a mirror can make all the difference.
The good news:
Caught early, skin cancer is one of the most treatable cancers we know.
Cervical Cancer
Almost all cervical cancers are caused by the human papillomavirus virus (HPV), a common virus that spreads through sexual contact. Smoking and immune disorders can also raise the risk.
Who’s at higher risk?
If you have a cervix, you need screening—period. Your risk goes up if you started having sex at a young age, have had multiple partners, multiple pregnancies, HIV, a compromised immune system, or if you smoke.
When to start screening:
By age 25, you should be seeing a gynecologist for Pap tests (every 1-3 years) and HPV tests (every 5 years). If you haven’t gotten the HPV vaccine, it’s not too late. You can get it until age 45, and it protects both women and men from HPV-related cancers.
The good news:
Thanks to the HPV vaccine, cervical cancer rates have dropped by 65% in the first generation of women who had access to it. That’s remarkable progress.
Breast Cancer
Breast cancer is what October is all about, and for good reason. It’s the second most common cancer in women, after skin cancer. One in eight women will develop breast cancer during their lifetime.
Who’s at higher risk?
Simply being female puts you at risk, and that risk increases as you get older. Genetics play a strong role, especially for BRCA1 and BRCA2 mutations (breast cancer associated genes). If breast or ovarian cancer runs in your family, if you started your period before 12 or went through menopause after 55, or if you have dense breasts, use hormone therapy, or struggle with obesity, your risk is higher. If any of this sounds like you, talk to your provider about starting to screen earlier.
When to start screening:
Start breast self-exams in your 20s. Most women worry they don’t know what they’re looking for, and that’s okay. Your gynecologist should be doing yearly manual exams starting in your 20s to help you understand what’s normal for your body. At age 40, start annual mammograms. We know the guidelines recently changed to every two years, but the Affordable Care Act requires insurers to cover yearly mammograms. That year can make a lifesaving difference. If you have dense breasts, you might need an additional ultrasound exam.
The good news:
Thanks to early screening, survival rates for breast cancer are increasing every year. When caught early, the five-year survival rate is 99%.
Colon Cancer
Colon cancer is the fourth leading cause of cancer deaths in the U.S., but it’s also one of the most preventable. Colon cancer has become more common among younger people in recent years. We don’t fully understand why, but it means screening at the right age matters more than ever.
Who’s at higher risk?
Family history is huge here. If your parents, siblings, aunts, uncles, or grandparents had colorectal cancer or certain types of polyps, your risk goes up. Inflammatory bowel diseases like ulcerative colitis or Crohn’s increase your risk.
Age is a factor, too. Native Americans have the highest rates of colorectal cancer in the U.S., followed by African Americans. People of Ashkenazi Jewish descent have one of the highest rates in the world. Obesity and a low-fiber, high-fat diet also increase your risk.
When to start screening:
Most people should begin screening at age 45, or 10 years before the age a close relative was diagnosed.
Your best option is a colonoscopy every 5–10 years. It not only finds cancer, but it can also remove precancerous polyps during the same procedure. Yes, it takes a little prep and a half-day off work, but you’ll rest easy knowing you did something that truly prevents cancer.
There are stool and blood tests that seem easier, but they’re less accurate and may still lead to a colonoscopy later, often with less insurance coverage.
The good news:
When caught early through screening, the five-year survival rate for colon cancer is 90%.
Lung Cancer
Lung cancer takes more lives than any other cancer, but early detection makes a world of difference. The problem? Lung cancer screening isn’t always top-of-mind for medical providers. You might have to ask for it. And it’s not always covered by insurance if you were never a smoker.
Who’s at higher risk?
If you’re a current or former smoker, this one’s for you. Previous radiation to your chest, like some breast cancer patients receive, also puts you at higher risk. So does a previous lung cancer diagnosis. Exposure to secondhand smoke, radon, or pollution increases risk, too.
When to start screening:
If you’re 50 or older and you’re a current or former smoker with at least a 20 pack-year history, you should be getting screened. Pack-year history sounds complicated, but it’s not. Just multiply the number of years you smoked by the number of packs per day. Two packs a day for 10 years equals 20 pack-years. One pack a day for 20 years equals the same. Screening involves a low-dose CT scan once a year. If you’ve never smoked, insurance may not cover it but talk to your provider about your specific risk factors.
The good news:
If caught early through screening, the 20-year survival rate for lung cancer is 81%. And your risk of developing lung cancer drops further every year after you quit smoking. That’s powerful inspiration to quit and stay smoke-free.
Prostate Cancer
This is one of the few cancers that only men can get. One in eight men will be diagnosed with prostate cancer during their lifetime—the same rate as breast cancer in women.
Who’s at higher risk?
All men face some risk, and that risk increases with age. African American men are at significantly higher risk and tend to develop it at younger ages. If prostate cancer runs in your family, especially if your father, brother, or son had it, your risk goes up considerably.
When to start screening:
Men should start talking with their provider around age 50, or age 45 if prostate cancer runs in the family, or if they’re African American.
Screening includes a PSA (prostate-specific antigen) blood test and a brief physical exam during your annual checkup. Your provider will feel your prostate to make sure it’s normal in size and shape. If you have a family history, start screening 10 years before the age your relative was diagnosed. PSA levels can be high for a variety of benign reasons. They don’t automatically mean cancer, but they tell your provider to look more closely.
The good news:
Prostate cancer is slow-growing and can be treated in a variety of ways. Screening is simple—no anesthesia, no radiation, virtually no side effects.
The Bottom Line
Cancer is scary. But getting screened shouldn’t be. These tests are simple, safe, and proven to save lives.
So yes, wear pink this month. Get your mammogram. Celebrate the progress we’ve made against breast cancer.
But also? Schedule that colonoscopy. Book your skin check. Ask your doctor about prostate or lung cancer screening.
This year, let’s make October about pink ribbons, but let’s also make it about you taking charge of your health, catching problems early, and living a long, healthy life.
Cancer screening saves lives.
But only if you actually do them.
We’re Here to Help
Not sure which screenings you need or when? Confused about what your insurance covers? You’re not alone. Guidelines change, and coverage can be hard to follow.
Amaze can help you create a personalized screening schedule based on your age, gender, family history, and risk factors.