
You Don’t Need to Wear a Mask in the Pool, But You Do Need to Know About the New Surging Variants!
And you thought all we had to worry about were deadly heat waves!
As we have in post-COVID summers past, we are seeing a serious spike in COVID cases. This year there are some obvious reasons for this:
- More people travel in the summer, and many are making up for previous summers.
- The heat is forcing some group activities indoors.
- It has been a long time since most of us have had a COVID-19 vaccine, so our immunity is waning.
The New Variants
Meet KP.1.1, KP.2, and JN.1. Their names are so dry and dull that they’ve gotten together and formed a cute variant group called FLiRT. The name “FLiRT” is based on the technical names for the variants’ spike protein mutations or the specific amino acid changes. Oops, here we are back to dry and dull.
What’s not so dull, but very annoying, is that the FLiRT group has developed an immunity to previous vaccines and previous variants. So, having had the virus and/or the vaccine is not very likely to protect you against one of these FLiRTs.
The New Symptoms
However, the FLiRT group is distinguishing itself from previous variations by adding gastrointestinal issues to the roster of COVID-19 symptoms. This could be another reason that the virus has been spreading so aggressively. People may mistake their COVID symptoms for food poisoning or a simple stomach bug, thus allowing them to innocently pass it along to others as soon as they are feeling better.
The good news is that, thanks to vaccinations and immunity from previous infections, the FLiRT variations are less likely than their predecessors to kill us or even send us to the hospital. But that is not true for those at high risk, like the elderly, children too young to be vaccinated, and people with compromised immune systems; this is the danger of the summer COVID spike. For high-risk people, COVID is just as deadly as it was in 2020, so it is well worth taking some COVID-era precautions.
Stop the Spread!
- Most of us have let our COVID test kits expire without replacing them. Now is a good time to pick up some kits and use them when you are experiencing anything that feels worse than a mild cold.
- You don’t have to skip the party, just try to avoid really crowded events. You don’t want to be anywhere where you will be 1-2 feet away from others for a prolonged period. Masks are always a good idea on airplanes.
- If you have a friend, relative, or co-worker who is at increased risk, consider increasing your protective measures and testing for COVID before being in contact with them. Wear masks during shows, concerts, and crowded events and wash your hands more frequently than usual.
- Keep up to date on the latest variants through the CDC, the NIH, or your favorite source of credible health information. Knowledge is power!
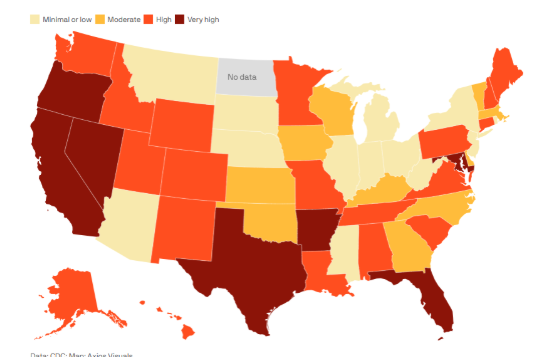
Are You in a Hot Zone?
Since the peak of the COVID crisis ended, people have been testing themselves with less frequency and are even less likely to go to the doctor or urgent care for a test when symptoms arise. With fewer test results available, to determine the hot zones for COVID, scientists test the wastewater across the country looking for areas with high levels of the virus. To find out where your state stands on the summer surge, check out the map below. The data was collected this month, and the darkest areas show the highest levels of the disease. The data was collected by the CDC and the map was created by Axios.
What To Do If You Get COVID-19 This Summer
Stay home. Get rest. Drink plenty of fluids. The basics haven’t changed much during the past four years, but three important things have:
COVID antivirals, like Paxlovid, are readily available. The key is to start taking the drugs during the first 3-5 days since your symptoms started. This is a good reason to have test kits at home. As soon as you test positive, call a medical professional to get a prescription.
Quarantine rules have been relaxed, but be smart. Several months ago, the CDC dropped its five-day isolation requirement. Now, the recommendation is that if you are diagnosed with COVID-19, you should stay home until you are fever-free for at least 24 hours and your symptoms are improving. This is pretty much standard for any virus. However, if you live or work with someone who is immunocompromised, you really should plan to keep your distance for 7-10 days.
If you are generally in good health, wait for the new vaccine to update your immunity. Although infectious disease experts have traditionally advised regular vaccine refreshers, this summer their advice is a bit different. Since the new variants are resistant to the old vaccines, you are much better off waiting for the new vaccine that will be widely available in September. That vaccine is designed to shoot down the FLiRTs and therefore will be much more effective.
A combination flu-COVID vaccine is in the works, but until that becomes available, experts say it is important to get a flu shot as well as the new COVID-19 vaccine. New research shows that the flu or a similar virus can trigger long-term COVID-19 in some who have long since recovered from the acute version.
The Bottom Line on the Summer COVID Surge
- Summer COVID surges are becoming common, and this summer’s extended heatwaves are making this year’s surge worse. Check the map above to see if you are in a hot zone.
- The latest FLiRT variants spread quickly and are resistant to old immunity, but are less lethal than their predecessors.
- Stay away from dense crowds and wash your hands often, particularly if you are in contact with anyone who is extremely vulnerable.
- The new strains often add gastrointestinal distress to their symptom rosters, so it may not be that extra burrito or “just a stomach bug.”
- If you test positive, discuss the option of taking an anti-viral with a healthcare professional. You should take it within 3-5 days of the onset of symptoms.
- Wait for the new vaccine and get one when it is available.