
Know the Symptoms. Have a Plan. Your Brain Will Thank You!
Imagine this: You’re enjoying lunch with a friend when suddenly, she can’t seem to find her next word and seems frozen in place for a long moment. Maybe the moment passes, one of you says, “That was weird,” and you carry on. Maybe she ends the lunch because she feels like she is “coming down with something.”
If you are younger than age 65, chances are you won’t be thinking the incident could be signaling a stroke. And that might be a costly mistake.
The fact is that the frequency of strokes in people between 18 and 65 years old has been increasing significantly during the past decade. It’s not so surprising when you consider that related issues like obesity, diabetes, and hypertension have also been increasing during that time.
While we all know that we should be eating healthier and exercising more, most of us are less clear about what could be happening in our brains during a stroke and how to tell if you are having one or even if you will have one soon. So read on for information that could save your brain functionality or even your life.
What Exactly is a Stroke?
There are two types of strokes, ischemic and hemorrhagic, and both result from an injury to a blood vessel that limits blood flow to part of the brain. Without the steady supply of oxygen and nutrients that blood vessels carry, brain cells start to die—at an alarming rate of 1.9 million cells per minute! The resulting damage can leave you unable to move, speak, feel, think, see, or even recognize other people.
A hemorrhagic stroke occurs when a blood vessel in the brain leaks or ruptures. If the bleeding is heavy enough, it creates a mass of accumulated blood called a hematoma, which compresses nearby brain tissue. Under this pressure, oxygen and nutrients can’t reach brain cells, which die as a result. A hemorrhagic stroke is a little less insidious than an ischemic stroke because its symptoms are severe enough to force most of us to seek help.
Common Symptoms:
- Severe Headache: Often described as the “worst headache of my life,” this is a hallmark of hemorrhagic stroke due to the bleeding in or around the brain.
- Nausea and vomiting: Common due to the pressure build-up from the bleeding.
- Sudden loss of consciousness: This can occur if the bleeding causes a rapid increase in intracranial pressure.
- Seizures: Sometimes, bleeding in the brain can trigger a seizure.
Ischemic strokes are by far the most common, accounting for about 87% of all strokes. It is also much harder to identify. An ischemic stroke occurs when an artery supplying the brain is blocked by a blood clot. Ischemic strokes behave like heart attacks in the brain.
Think of a blocked pipe—this is essentially what happens during an ischemic stroke. Blood can’t reach a part of the brain, and that brain tissue begins to die.
Common Symptoms:
- Sudden numbness or weakness, particularly on one side of the body.
- Confusion, trouble speaking, or difficulty understanding speech.
- Sudden trouble seeing in one or both eyes.
- Dizziness, loss of balance, or lack of coordination.
- Sudden severe headache (less common than in hemorrhagic stroke).
As you can see, these symptoms, especially if you suffer only one or two, can easily be mistaken for something else like stress, a pinched nerve, the flu, a stomach bug, a sinus infection, and even the momentary dizzy feeling you get when you stand up too fast. But taking too long to recognize a stroke can have terrible consequences.
Are You at High Risk?
The higher your stroke risk, the more critical it is for you to learn the symptoms of a stroke and make a plan “just in case.”
- Women are at higher risk than men of both having a stroke and dying from a stroke.
- Among younger adults, Black people are four times as likely to have a stroke than white people, while Hispanics are twice as likely.
- If someone in your immediate family has had a stroke, your risk is about 30% higher than it would be otherwise. Having a parent who had a stroke before age 65 triples your risk.
- Of course, conditions like obesity, diabetes, hypertension, high cholesterol, alcohol/drug abuse, and smoking—the ones that raise your risk of many catastrophic diseases—significantly raise your risk of having a stroke.
- If you have had a TIA, you have a one-in-three chance of having a stroke.
TIA – The Paul Revere for Strokes
In grade school, most of us learned about the legendary Paul Revere, who rode through Boston in the middle of the night warning, “The British are coming!”
Similarly, TIAs, or transient ischemic attacks, are our bodies’ way of announcing that a stroke may be coming. According to the American Heart Association, almost twenty percent of people who experience a TIA will have a stroke within three months—and half of those strokes will occur within a few days. About one-third of people who have a TIA go on to have a stroke within a year!
A TIA is a temporary blockage in a blood vessel supplying the brain, sometimes known as a “mini-stroke.” Because the blockage is temporary, TIA symptoms are milder than stroke symptoms and often pass within minutes. This makes it incredibly easy to miss a TIA completely. In the situation described at the top of this article, our friend most likely had a TIA. If she doesn’t seek specific medical care, she has a good chance of having a full-blown stroke in the near future.
TIAs usually last several minutes to a few hours, although the symptoms may last up to 24 hours. The longer the duration of symptoms, the higher the risk for brain damage. If symptoms, however mild, continue beyond 24 hours, it is no longer a TIA but a full-blown stroke, and some brain tissue death has likely occurred.
Reducing Your Stroke Risk After TIA
The good news is that seeking medical help immediately after a TIA will help you reduce your risk of being part of the one-third who will have a stroke within a year. Generally, anyone who has a TIA should take an aspirin and have an MRI within 24 hours. Aspirin is an antiplatelet medication, meaning it prevents blood cells called platelets from clumping together to form a clot, and an MRI will determine the location of the blockage and the risk of an impending stroke.
It’s also quite likely that a doctor will prescribe longer-term medication to prevent clotting and lower both blood pressure and cholesterol right away. Research suggests that if you start these preventive treatments within one day of a TIA, you are far less likely to have a stroke during the following 90 days than if you wait a few weeks to start the preventive measures.
Speed Counts When You Have a Stroke
The importance of identifying and treating a stroke as soon as possible can’t be stressed enough. The goal of treatment is to restore blood circulation (or to stop the bleeding) before brain tissue dies. The time frame for reaching this goal is frighteningly slim. Current treatments to prevent brain cell death begin losing their effectiveness within 60 minutes of the onset of symptoms, so every minute counts. For every minute lost during a stroke, nearly 2 billion brain cells are at risk. Quick action can save lives and limit brain damage.
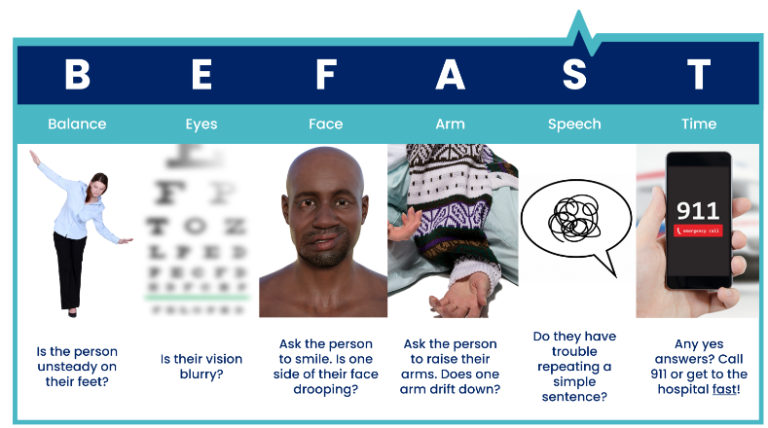
BE FAST: A Lifesaving Acronym
When it comes to strokes, every second counts. The acronym BE FAST was devised by the American Stroke Association and enhanced by neurologists to help you quickly identify symptoms of a stroke and act fast:
- Balance: Sudden loss of balance or unsteady walking.
- Eyes: Double vision or loss of vision.
- Face: The face may droop on one side.
- Arms: One arm may be frozen or numb.
- Speech: Speech may become slurred, confused, or difficult to understand.
- Time: Call 911 immediately.
PLAN
It’s not an acronym, but it is a good idea. If you are at a higher-than-average risk of having a stroke (and even if not), prepare for an emergency by posting important phone numbers somewhere clearly visible and keep them easily accessible in your Amaze app. These should include the numbers of your doctor and a relative or close friend who should be contacted in case of an emergency. You should also have handy a current list of prescription medications (especially any blood thinners) and other medications you take, as well as a brief medical history, to take to your chosen hospital in the event of a stroke. There are places to store all this information in your Amaze app.
The Bottom Line on Strokes
Strokes are becoming more common among people younger than 65. Your chances of having a stroke depend on various risk factors—some that you can change and some that you can’t. The chances of you and anyone else surviving a stroke with maximum brain function will depend on how fast you identify stroke symptoms and get medical help. Memorize the symptoms of a stroke with the acronym BE FAST. Assess your stroke risk and plan for the worst-case scenario. You’ll save millions of brain cells and your quality of life that way.