
September is Suicide Prevention Awareness Month – But This Info is Worth Knowing Every Month
Suicide is a difficult topic, but it becomes increasingly important with each passing year. During the last decade, the number of suicides in the US has increased each year (with a slight, inexplicable dip during the worst COVID years 2020 and 2021). Since its introduction in July 2022, the 988 Lifeline has received almost 5 million contacts, including almost one million from the Veteran’s Crisis Line.
Perhaps the best way for each of us to help reverse the trend is to understand the risk factors for suicide, recognize common suicide signaling, and learn ways to help someone in crisis. The information that follows may save lives.
Risk Factors
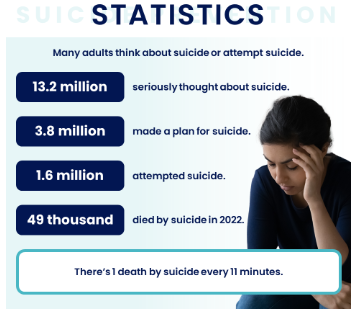
Lets start with some recent statistics:
- Indigenous Americans (American Indian and Alaskan Native) have the higest suicide rates, followed by Non-Hispanic White, Native Hawaiian or Other Pacific Islanders.
- Rates are higher among Americans living in rural communities than those in more populated areas.
- Males are four times as likely to commit suicide than women. They make up 50% of the population but account for 80% of all US suicides.
After race, location, and gender, the major risk factors for suicide are mental health disorders, substance abuse, physical illness or pain, and major life events.
Mental Health Disorders
- Depression: Individuals may experience persistent sadness, loss of interest in activities, and feelings of worthlessness. For example, a person may lose interest in hobbies they once loved or express feeling like a being a burden to others.
- Anxiety: Constant worry, panic attacks, or feelings of impending doom can overwhelm a person. They might avoid situations that cause anxiety or express concerns about things others might find minor.
- Post-Traumatic Stress Disorder (PTSD): This can follow exposure to traumatic events (war, assault, accidents). For instance, a veteran who struggles with flashbacks or nightmares may feel like they can’t escape the past.
- Bipolar Disorder: Sudden shifts from extreme highs (mania) to deep lows (depression) can lead to feelings of instability and hopelessness. Someone in a manic phase might make impulsive decisions, while during a depressive phase, they could feel their situation is unchangeable.
Substance Abuse
- Excessive use of alcohol or drugs can worsen mood disorders and lower inhibitions, making someone more likely to act on suicidal thoughts. For instance, a person might start drinking heavily after the end of a relationship and feel even more isolated, intensifying thoughts of self-harm.
Chronic Pain or Serious Illness
- Conditions like cancer, chronic pain (e.g., fibromyalgia, migraines), or disabilities can lead someone to feel hopeless or that their quality of life is diminishing. Someone with a long-term illness might say, “I don’t want to be a burden to my family anymore” or “This pain will never go away.”
Major Life Stressors
- Loss of a loved one: Death, divorce, or breakups can leave a person feeling isolated or heartbroken. For example, someone might not see a way forward after losing a spouse, saying, “I don’t know how to go on without them.”
- Job loss or financial struggles: The sudden loss of employment or financial instability can trigger a sense of failure. They might express thoughts like “I’ve failed my family” or “They’d be better off without me.”
- Bullying or harassment: Teens or adults experiencing ongoing bullying or discrimination (in school, the workplace, or due to gender, sexuality, or race) may start feeling like there’s no escape.
Isolation
- Social disconnection: Lack of close relationships or support networks can lead to intense feelings of loneliness. A person might avoid social interactions or withdraw from friends and family, expressing thoughts like “No one would even notice if I was gone.”
Previous Suicide Attempts
- A history of attempting suicide increases the risk of future attempts. If someone has attempted before, they may be more vulnerable, especially during high-stress periods.
Warning Signs – When to Help
Warning Signs: Behaviors or statements that may indicate someone is at immediate risk.
- Direct statements: A person might directly express their suicidal thoughts or intent. Examples include:
- “I want to die.”
- “I’m going to kill myself.”
- “I can’t take this anymore.”
- “Everyone would be better off if I weren’t here.”
- Indirect statements: These are more subtle and can hint at suicidal thinking without explicitly stating it. Examples include:
- “I just can’t see any way out.”
- “What’s the point of going on?”
- “I feel like I’m a burden to everyone.”
- “I won’t be around much longer.”
- “I’m tired of life.
Behavioral Changes
- Withdrawal from social activities: If someone who was previously social starts avoiding friends, family, or activities they once enjoyed, this could be a red flag. For example, a normally outgoing person stops answering texts or cancels plans without explanation.
- Increased substance use: A person may begin using alcohol or drugs more frequently or heavily. For instance, someone may turn to alcohol to cope with stress, saying, “It helps me forget for a while.”
- Giving away possessions: A sudden decision to give away valuable or sentimental belongings can indicate that someone is preparing for death. For example, they might offer up personal items like a favorite book or treasured keepsake, saying, “I won’t need this soon.”
- Sudden mood improvements: If a person who was recently very depressed suddenly appears calm or happy, this might be a sign they’ve made the decision to take their life. For example, after weeks of seeming despondent, they might say, “Everything will be fine soon.”
- Neglecting personal appearance: Changes in self-care, such as neglecting hygiene, not eating, or wearing the same clothes for days, can indicate a loss of interest in life.
Mood Changes
- Severe mood swings: A person may go from extreme agitation or anger to sudden calmness or detachment. For example, someone might lash out at loved ones, then later seem distant or unresponsive.
- Despair or hopelessness: Expressions of hopelessness, such as “Nothing will ever get better,” can indicate that a person no longer sees a future for themselves.
- Agitation and restlessness: A person might seem constantly on edge or unable to relax. They may pace, struggle to focus, or have trouble sleeping, which could signify inner turmoil.
Planning or Prepping for Death
- Searching for means: If someone is researching methods to end their life, such as looking up information about pills, weapons, or other methods, this is an urgent warning sign.
- Writing about death: Someone may start writing or talking about death frequently. They might leave notes or messages on social media that hint at their intent.
- Making final arrangements: Organizing personal affairs, writing a will, or making funeral arrangements can be signs that someone is planning for their death. For example, someone may say, “I need to get my things in order.”
What to Do When You See Warning Signs
- Reach Out and Start the Conversation
Be direct and ask about suicide: It can feel scary to ask someone directly if they’re thinking about suicide, but it’s one of the most important things you can do. People often fear that asking about suicide might “put the idea in their head,” but research shows that asking can help them feel understood and supported.
- How to ask: You can say something like, “I’ve noticed you’ve been struggling lately. Have you been thinking about hurting yourself?” or “Are you feeling like you don’t want to live anymore?”
- Why this matters: Being direct opens the conversation and shows that you care about them. It also gives the person an opportunity to talk about their feelings instead of keeping them bottled up.
- Listen Without Judgement
Be present and just listen: Once you’ve asked the question, let them talk. Don’t interrupt or try to immediately “fix” things. Sometimes, just letting someone express their pain is incredibly helpful.
- How to do this: Try communicating, “I’m here for you, and I want to understand what you’re going through.” It’s important not to minimize their feelings with phrases like, “It’s not that bad,” or “You’ll get over it.”
- Why this matters: Feeling heard and not judged can make a big difference to someone who feels isolated. Your willingness to listen can help them feel less alone.
- Show You Care
Offer empathy and support: Let them know that you care and that their life matters to you.
- What to say: Simple phrases like “You’re really important to me” or “I want to help you through this” can go a long way.
- Why this matters: People thinking about suicide often feel like no one cares about them or that they are burdensome. Reminding them that they’re loved and valued might make them reconsider their thoughts about taking their own life.
- Encourage Them to Seek Professional Help
Suggest they talk to a professional: While your support is important, it’s essential that they speak to a mental health professional who can offer the right guidance.
- How to do this: You can say, “I think it would really help to talk to a counselor or therapist about what you’re going through.” Offer to help them make the call or even go with them if they’re scared.
- Why this matters: Mental health professionals are trained to help people navigate suicidal thoughts and emotions. They can offer therapy, treatment, or other forms of help that you may not be able to provide.
- Remove Immediate Dangers
Keep them safe: If you believe someone is in immediate danger of harming themselves, it’s crucial to take steps to remove any means they might use to hurt themselves.
- What to do: This might mean removing things like pills, sharp objects, or firearms from their environment. You can say something like, “Let’s move these things for now, just to be safe.”
- Why this matters: People who are feeling suicidal can act impulsively and one extra step can be lifesaving. If the means to harm themselves are less accessible, it can reduce the risk of them following through.
- Stay with Them if They’re in Crisis
Don’t leave them alone: If someone is actively suicidal—meaning they have a plan or intent to harm themselves—stay with them until they can get help.
- What to do: Call emergency services or a crisis hotline (like 988 in the US) and let them know that the person is at risk of suicide. While waiting, sit with them, talk to them, and offer calm reassurance. Don’t leave them by themselves.
- Why this matters: Staying with someone in a crisis can prevent them from acting on their suicidal thoughts. You can be the support they need until professionals can step in.
- Follow Up After the Crisis
Check in on them regularly: Even after the immediate danger has passed, it’s important to keep checking in on your friend or loved one.
- What to do: Reach out with texts or phone calls to let them know you’re still thinking about them and that you care. You can say, “Hey, I just wanted to check in and see how you’re doing today.”
- Why this matters: Regular follow-up shows the person that they’re not alone, and that your support was not just a one-time event. This helps them feel supported in the longer term and can reduce their sense of isolation.
Survivor’s Guilt – When You Have Lost Someone to Suicide
Survivor’s guilt is a deeply painful and complex emotion that often arises after losing someone to suicide. People affected by suicide may feel responsible, wonder if they could have prevented the death, or feel guilty for being alive while their loved one is gone. Handling these emotions is difficult, but there are steps you can take to cope with the loss and avoid falling into your own despair.
Acknowledge Your Feelings
- Understand that survivor’s guilt is normal: It’s common to feel a range of emotions after a loved one’s suicide, including guilt, anger, confusion, and sadness. Recognizing that these feelings are natural can be the first step toward healing.
- Allow yourself to grieve: Grieving is a crucial part of healing. You may feel intense emotions, and that’s okay. Don’t suppress or ignore these feelings—give yourself permission to feel them.
- Avoid self-blame: It’s common for survivors to ask themselves questions like, “What could I have done?” or “Why didn’t I see this coming?” It’s important to remember that suicide is a complex issue, and the choice to end one’s life is rarely due to one single factor. Blaming yourself won’t change the outcome, and no one person is responsible for someone else’s suicide.
Seek Support
- Talk to someone you trust: Sharing your feelings with a close friend, family member, or counselor can help you process your emotions. You don’t have to carry this burden alone.
- Professional therapy: If feelings of guilt or despair are overwhelming, it’s important to seek professional help. Therapists can help you process grief, work through feelings of guilt, and prevent those feelings from spiraling into deeper depression. Grief counseling, in particular, is designed to help survivors process loss.
- Connect with the Alliance of Hope: The Alliance of Hope for Suicide Loss Survivors was created by survivors for survivors and provides healing support and other services through an online forum that operates like a 24/7 support group.
Accept What You Cannot Control
- Understand the limits of control: One of the most difficult aspects of losing someone to suicide is feeling that you might have been able to prevent it. However, it’s important to recognize that, while you may have cared deeply for the person, you could not control their actions or mental health. People who take their own lives are often suffering in ways that are invisible to those around them, and their decision is usually the result of complex factors that no one person could change.
- Release the need for answers: Suicide often leaves behind unanswered questions, and that can be one of the most painful aspects of grieving. You may never fully understand why your loved one made that decision, and accepting the ambiguity can be a difficult but necessary part of the healing process.
Recognize Warning Signs in Yourself
- Take care of your physical health: Grief can be exhausting, and it’s easy to neglect physical well-being. Make sure you’re eating regularly, getting enough sleep, and incorporating physical activity to manage stress.
- Monitor your mental health: It’s important to be aware of how your grief is affecting your own mental health. Feelings of guilt and despair can become overwhelming, especially in the aftermath of a traumatic loss. If you find yourself experiencing persistent hopelessness, withdrawal, or suicidal thoughts, it’s crucial to reach out for help immediately.
Please remember, no matter how you are feeling, there is always help available.
- The National Alliance on Mental Illness (NAMI) is the largest grassroots mental health organization in the U.S., offering support, education, and advocacy for millions of Americans affected by mental illness.
- If you need to talk, the 988 Lifeline is here 24/7, every day of the year. Whether you’re dealing with mental health struggles, emotional distress, substance use concerns, or just need someone to listen, you can call, text, or chat with a compassionate counselor at the 988 Lifeline.