
September is Suicide Prevention Awareness Month,
But This Info is Worth Knowing Every Month
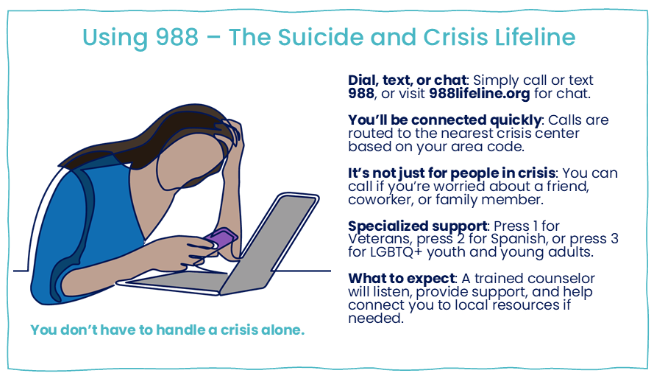
Suicide is a difficult topic, but it becomes increasingly important with each passing year. During the last decade, the number of suicides in the US has increased each year (with a slight, inexplicable dip during the worst COVID years 2020 and 2021). Since its introduction in July 2022, 988 has received almost 18 million contacts.
Perhaps the best way for each of us to help reverse the trend is to understand the risk factors for suicide, recognize common suicide signaling, and learn ways to help someone in crisis. The information that follows may save lives.
Risk Factors
Suicide doesn’t have one single cause — it’s usually the result of many factors coming together. Here are the most common risks:
- Demographics: Highest among Indigenous Americans, followed by non-Hispanic Whites and Native Hawaiian/Pacific Islanders. Rates are higher in rural communities. Men die by suicide at four times the rate of women.
- Mental health conditions: Depression, anxiety, bipolar disorder, and PTSD all increase risk.
- Substance use: Alcohol and drug misuse can worsen mood disorders and lower inhibitions.
- Physical illness or pain: Chronic conditions or major diagnoses can fuel hopelessness.
- Life stressors: Loss, divorce, financial strain, bullying, or harassment may intensify despair.
- Isolation and disconnection: Lack of close support networks or withdrawal from relationships.
- History of attempts: Past attempts remain one of the strongest predictors of future attempts.
Warning Signs – When to Help
Warning Signs: Behaviors or statements that may indicate someone is at immediate risk.
- Direct statements: A person might directly express their suicidal thoughts or intent. Examples include:
- “I want to die.”
- “I’m going to kill myself.”
- “I can’t take this anymore.”
- “Everyone would be better off if I weren’t here.”
- Indirect statements: These are more subtle and can hint at suicidal thinking without explicitly stating it. Examples include:
- “I just can’t see any way out.”
- “What’s the point of going on?”
- “I feel like I’m a burden to everyone.”
- “I won’t be around much longer.”
- “I’m tired of life.”
Behavioral Changes
- Withdrawal from social activities: If someone who was previously social starts avoiding friends, family, or activities they once enjoyed, this could be a red flag. For example, a normally outgoing person stops answering texts or cancels plans without explanation.
- Increased substance use: A person may begin using alcohol or drugs more frequently or heavily. For instance, someone may turn to alcohol to cope with stress, saying, “It helps me forget for a while.”
- Giving away possessions: A sudden decision to give away valuable or sentimental belongings can indicate that someone is preparing for death. For example, they might offer up personal items like a favorite book or treasured keepsake, saying, “I won’t need this soon.”
- Sudden mood improvements: If a person who was recently very depressed suddenly appears calm or happy, this might be a sign they’ve made the decision to take their life. For example, after weeks of seeming despondent, they might say, “Everything will be fine soon.”
- Neglecting personal appearance: Changes in self-care, such as neglecting hygiene, not eating, or wearing the same clothes for days, can indicate a loss of interest in life.
Mood Changes
- Severe mood swings: A person may go from extreme agitation or anger to sudden calmness or detachment. For example, someone might lash out at loved ones, then later seem distant or unresponsive.
- Despair or hopelessness: Expressions of hopelessness, such as “Nothing will ever get better,” can indicate that a person no longer sees a future for themselves.
- Agitation and restlessness: A person might seem constantly on edge or unable to relax. They may pace, struggle to focus, or have trouble sleeping, which could signify inner turmoil.
Planning or Prepping for Death
- Searching for means: If someone is researching methods to end their life, such as looking up information about pills, weapons, or other methods, this is an urgent warning sign.
- Writing about death: Someone may start writing or talking about death frequently. They might leave notes or messages on social media that hint at their intent.
- Making final arrangements: Organizing personal affairs, writing a will, or making funeral arrangements can be signs that someone is planning for their death. For example, someone may say, “I need to get my things in order.”
What to Do When You See Warning Signs
What You Can Do
- Ask directly. It doesn’t plant the idea — it shows you care.
- Listen without judgment. Sometimes being heard is the first lifeline.
- Show you care. Let them know they matter.
- Encourage professional help. Offer to connect them with a counselor or doctor.
- Remove immediate dangers. Secure medications, weapons, or other means.
- Stay with them in crisis. If they’re at risk, call 988 or 911 and don’t leave them alone.
- Follow up. Check in regularly, even after the crisis has passed.
Survivor’s Guilt — When You Have Lost Someone to Suicide
Survivor’s guilt is a deeply painful and complex emotion that often arises after losing someone to suicide. People affected by suicide may feel responsible, wonder if they could have prevented the death, or feel guilty for being alive while their loved one is gone. Handling these emotions is difficult, but there are steps you can take to cope with the loss.
- Acknowledge Your Feelings
- Understand that survivor’s guilt is normal: It’s common to feel a range of emotions after a loved one’s suicide, including guilt, anger, confusion, and sadness. Recognizing that these feelings are natural can be the first step toward healing.
- Allow yourself to grieve: Grieving is a crucial part of healing. You may feel intense emotions, and that’s okay.
- Avoid self-blame: It’s common for survivors to ask themselves questions like, “What could I have done?” or “Why didn’t I see this coming?” It’s important to remember that suicide is a complex issue. Blaming yourself won’t change the outcome, and no one person is responsible for someone else’s suicide.
- Seek Support
- Talk to someone you trust: Sharing your feelings with a close friend, family member, or counselor can help you process your emotions. You don’t have to carry this burden alone. Survivors can call 988 too.
- Professional therapy: If feelings of guilt or despair are overwhelming, it’s important to seek professional help. Amaze can help you find what you need. Grief counseling, in particular, is designed to help survivors process loss.
- Recognize Warning Signs in Yourself
- Take care of your physical health: Grief can be exhausting, and it’s easy to neglect physical well-being. Make sure you’re eating regularly, getting enough sleep, and incorporating physical activity to manage stress.
- Monitor your mental health: It’s important to be aware of how your grief is affecting your own mental health. Feelings of guilt and despair can become overwhelming, especially in the aftermath of a traumatic loss. If you are feeling that way, it’s crucial to reach out for help.
The Bottom Line
Suicide prevention isn’t just for professionals. It’s something we can all take part in by noticing changes, asking questions, and connecting people to help. You don’t have to have all the answers; you just have to show up.